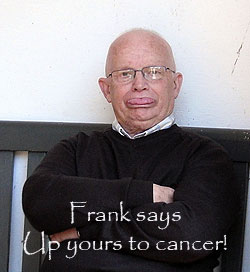
One man's cancer.
 I don't intend to write this as a guide to coping with cancer. This is just my
story & my thoughts, going through what is a life changing experience.
I don't intend to write this as a guide to coping with cancer. This is just my
story & my thoughts, going through what is a life changing experience.
I know that in March of 2010, I felt as fit as a horse. I had returned from a trip to Hutton le Hole in North Yorkshire and everything was working great!
What seems to happen is there are small changes in your body & you just think its old age/natural changes that are affecting you. After all I had passed 70 & thought I was immortal. I'd heard men's prostate enlarges with age & thought it was all part of the process of becoming a senior citizen.
On 15th April I had a general health check & told my doctor that I was having
increasing problems passing water over the last couple of weeks. He moved very
quickly & had a PSA (Prostate-specific antigen) test done on my blood
sample, suspecting prostate cancer. As it happened, it should have returned a
reading of about 4 & it turned
out to be 24. (whatever that means!). His immortal words were, "If I had to have
cancer, I'd choose the prostate because its easy to fix". Little did either of
us know what was really happening.
This is the point you have to mention the NHS. Although things could never be described as perfect, my doctor (Dr. Ahmad of Croston), every nurse, consultant/doctor, helper, tea lady, cleaner or admin wallah were all very good. I cannot praise them enough. Admittedly, some were outstanding, but all of them did their best most of the time.
Although my wife & I were separated by then, she took the news well, if shocked. She had already had bad experiences with cancer via her mother, sister & cousin, all of whom had died with it. She has never been less than an understanding support though all of it. I am also blessed with good friends & a positive outlook about the whole thing.
Things seemed to move swiftly then. You got to know your doctor very personally as he had to give you the finger up the jacksie test, to feel the size of your prostate. (No foreplay, not even a kiss, but now at least he calls me Frank!) By the 26th I got an appointment to see Mr. Javle (Pronounced Jarvalay) at Chorley hospital. It was the start of so many tests. This time it was blood pressure, pee flow tests & another rectal examination. It was his opinion too, that I had prostate cancer & needed a biopsy. The actual time to see the consultant, have the checks, book an appointment and pick up three antibiotic tablets was very practical & fast, but the time hanging around seems massive. I went in at 10:30 & came out at 1:30. Take my word for it, allow lots of time for everything in hospital!
For the biopsy, you are required to lay on your side, an instrument is passed up your bottom & they cut away lots of samples from the prostate. I was assured it was uncomfortable, but not painful. As if I believed that! On the 28th I turned up at the Longton day case unit at Chorley hospital at 2:30. I filled in forms from which a student nurse completed a computer sheet. I hung around & then undressed into hospital gown, a dressing gown & slippers. Nurse said I needed my pee testing to check that I was OK for the procedure & after being lead into a room, told I MAY have a water infection as there were Leucocytes in my pee and that I could not have the test! Leucocytes are usually an indication of an infection, so as I was going to have bits cut off my prostate, I couldn't risk any other form of infection. Of course you build up the stress levels waiting for the unpleasantness & then you're sent home! Its as much fun as going to the dentist!
Then started the real fun & games!
For a couple of days I continued to kid myself I wasn't having trouble passing
water, and nothing was getting worse, convincing myself all this was just a temporary blip. By 4am
on the 1st of May I realised I certainly
wasn't going to pass any water. I waited to see if getting up & moving
around would release it but decided to go straight to A & E at Chorley,
especially as we were now over the bank holiday period. This is where I first became aware of
the word "Retention". Its painful, frustrating, embarrassing & somewhat
frightening.
It was murder just hanging around, bouncing from foot to foot & trying to
use the toilet when it just wouldn't flow at all.
They were very nice staff, very understanding, but they were coping with
anything & everything that was thrown at them. There is a thing called triage, a process for sorting injured
people into groups based on their need for, or likely benefit from, immediate
medical treatment. Triage is used in hospital emergency rooms, on battlefields,
and at disaster sites when limited medical resources must be allocated. I knew
there were guys there in bad condition, but I was in a continuous expectation
that I would explode .... painfully!
 A Dr. Patel was very good, lots of checks & questions, but we both knew he had to
fit a catheter. Oh how I learned to dread the word & slowly learned to hate the
bloody things! Nevertheless its a huge relief when this long plastic tube goes
in through your penis, to the bladder, & all that pain subsides away. It was done
very well with no pain & not a lot of discomfort. All a catheter does is
drain the bladder into a plastic bag continuously, with no effort. There is a small balloon
that has to be inflated at the end. This is what prevents it from coming
out of the bladder.
A Dr. Patel was very good, lots of checks & questions, but we both knew he had to
fit a catheter. Oh how I learned to dread the word & slowly learned to hate the
bloody things! Nevertheless its a huge relief when this long plastic tube goes
in through your penis, to the bladder, & all that pain subsides away. It was done
very well with no pain & not a lot of discomfort. All a catheter does is
drain the bladder into a plastic bag continuously, with no effort. There is a small balloon
that has to be inflated at the end. This is what prevents it from coming
out of the bladder.
A third test was done of my water. (the staff kept saying an infection in the water
can produce the same effects).
There was a lot more hanging around, but eventually the decision was made to send
me to Ward 10, Surgical assessment at The Royal Preston hospital (Used to be
called PRI). So I got a ride in an ambulance, in a chair, half dressed & carrying
my pee in what became known as my handbag! Its amazing how careful a man can be
with a thing up his willie & a bag full of water hanging on the end! The
ambulance men are always so nice, cheerful & helpful.
Again there were lots of questions in ward 10, form filling & tests for blood pressure,
pulse & temperature.
A house doctor checked me over & then allocated me to Ward 15 bay 5 on the 4th
floor. Once again all the same tests were done, plus an injection in the belly for DVT
prevention.
The first night I was up very late. The tablets were given, & the Obs
(patient observations) taken at 23:15 instead of the usual 10pm. Obs always
consist of blood pressure, temperature, pulse, "are you in any
pain? Do you feel sick?".
With the anxiety, the noise, other ill patients & the lights on all the time,
it was not an easy first night. Sleeping on your back, with tubes wrapped round
your legs & the occasional vaguely irritating catheter, it felt strange,
the first
hospital admittance of my life. At least I wasn't in pain anymore & they were fixing things.
There was a gentle wakening at about 7 ish as the hospital starts up. The Obs,
the pill run and breakfast always start the day.
By 10 am the doctors come round. Now this is a teaching Hospital ... every one
comes mob handed. There are consultant doctors, student doctors & senior nursing staff
all talking between themselves. You're under observation and asked questions,
but seldom does anyone actual answer a direct question (“is my water infected?”).
No one seems to know. Is this because they haven't got the information or they
are training people & its up to the juniors to find this out & they are
questioned later?
At least they made a decision on giving me tablets (Tamurex to relax the bladder &
enable the flow to be easier).
On the next day, 3rd May, I had my second tablet. You realise from the guys
who have been here some time that you seldom see the same doctor twice. No one tells
you who is the boss, you gather that he/she is the gaffer who asks questions &
all the others write stuff down. The only vague information I got was that the catheter
would/may/could come out today or tomorrow for a TWOC (test without catheter).
Bay 5 is next to the ladies toilets & it's quite a walk to the gents. There's no
plug in any basins, no mixer taps & a sign saying “this water is very hot” (well
it may GET hot but it wasn't when I used it!). Its amazing what a struggle it was to manage
getting out of bed, get on a dressing gown & slippers. Then I had to
carry my wash bag, towel, & bag of
pee, that was hanging on a metal frame, up & down the long corridor! I moved SO
slowly! I was so conscious that my willie was attached
to everything. It all seems to swing & bang around. Just learning where
to put everything & trying to wash is a difficult learning curve. There is
bugger all dignity available but luckily most of us are in the same boat and it
doesn't bother them … but it takes
some getting used to!
Very early on in the morning of the 5th. I got the sensation of not being able
to pass water. Now with a catheter in, that shouldn't happen! I was getting very
uptight by 6am. No one was around, the other lads were asleep & I couldn't see a
way of calling nurse. Anyway I found a button you pulled “emergency call” …....
it woke up the entire place … it was for nurses only! My god they react quickly.
Suddenly lots of staff arrived at my bedside!
Somehow I wasn't shot or hung! They seemed to realise I'd been in for some time &
not been given my call button or shown how to use it!
Apparently the catheter just needed washing out, as blood & debris could block
it (another thing not explained). After
the nurse did something with a syringe, it all cleared up.
 I wouldn't say a bad word about the staff. They were all very good, but you got
the impression there was too much for them to do & you got to know things on a need know to
know basis as they occurred. Courteous, understanding, mostly cheerful, the staff
were very nice. They seemed to have too much to do. Especially all the writing.
Everything goes down on paper somewhere. There were just not enough
spare hands. Its also blindingly obvious that they have to prioritise! People in
trouble & needing attention get it first, the rest of us must exercise patience.
Perfectly understandable but a bit of a shock initially. You think you press the
bell to get more water & it will happen (“Don't forget, you have to drink at
least two litres a day to wash out your bladder, Frank”) … nope, they just promise to do their best & often
their best is quite outstanding. No wonder they are called Angels.
I wouldn't say a bad word about the staff. They were all very good, but you got
the impression there was too much for them to do & you got to know things on a need know to
know basis as they occurred. Courteous, understanding, mostly cheerful, the staff
were very nice. They seemed to have too much to do. Especially all the writing.
Everything goes down on paper somewhere. There were just not enough
spare hands. Its also blindingly obvious that they have to prioritise! People in
trouble & needing attention get it first, the rest of us must exercise patience.
Perfectly understandable but a bit of a shock initially. You think you press the
bell to get more water & it will happen (“Don't forget, you have to drink at
least two litres a day to wash out your bladder, Frank”) … nope, they just promise to do their best & often
their best is quite outstanding. No wonder they are called Angels.
By 11am the catheter was removed & the TWOC began. My god what a sense of freedom! There was no
pain taking it out. Relax, cough & bingo, the huge long tube was out!
There is a routine on the urological ward that all fluids going in & coming out
are strictly measured.
It took till 11:45 to give my first sample of 70 mm & 12:45 to give my second of
100mm. Each time the nurse wanted more samples but I got the impression she was
very busy & I wasn't an emergency. Lots of other things to do.
By 4pm I had produced 4 samples, then was taken for an ultra sound test to see if I was
emptying my bladder fully.
Pronounced OK, I was delayed with people saying they had to do thing like
release forms etc. By 5pm, Ian, my son, was there. We packed everything away & got out of there. This is the first time you realise that to leave hospital, you don't need
Angels, you need some over worked admin guy & the pharmacist! Fat chance! No one
leaves here quickly!
Return of the walking wounded
Now I was home the Tamurex continued to help the flow. It was not quick to start flowing but
it worked & I could cope.
I needed to ring the LDCU to arrange my next biopsy. It was fixed for 1:15 pm Wednesday the 12th.
Lots of people, with every
good intention, read the web, talk to their friends & give you lots of
information that overload your brain. Don't read the web! Stuff like this is SO
misleading, I think every cancer must be different! Your may find you mind playing tricks.
After going every two hours for an urgent but small pee, I got got very tired. I think I worried a lot & ended
up losing my temper with the fridge & being unreasonably emotional about
anything. In my case, tears were quick to come & there didn't seem to be anyway
to stop them. There seemed to be no end of small niggles & the word Cancer does
seem to be a way of curing constipation. Funnily enough, in my case the reverse
was true. After doctors giving me the finger test, I just seemed to end up with
irritating piles & a bunged up bum!
I needed someone to talk too. For once I was wise & saw my own Dr. Ahmad who
kindly reassured me it was normal to worry. 
 What I needed was a drop of normality, a treat, something to make me smile. So
I took my friend Cynthia and we went out for a light lunch at our friends at
Downham cafe. Keith &
Margaret run the cafe from Downham Post Office. They always greet you with a smile
and Margaret cooks
the best chips EVER and Keith has found he has a new talent as a cake baker! My
Great Grandfather was in Downham in the 1881 census. His cottage was just behind
their shop & its always been a special place for me. As it was May, we went
to another special place and inhaled the bluebells coming up in Spring Wood in the
sunshine at Whalley.
I felt good, but as this goes on, there would no doubt be worse days until I
can learn to cope better.
What I needed was a drop of normality, a treat, something to make me smile. So
I took my friend Cynthia and we went out for a light lunch at our friends at
Downham cafe. Keith &
Margaret run the cafe from Downham Post Office. They always greet you with a smile
and Margaret cooks
the best chips EVER and Keith has found he has a new talent as a cake baker! My
Great Grandfather was in Downham in the 1881 census. His cottage was just behind
their shop & its always been a special place for me. As it was May, we went
to another special place and inhaled the bluebells coming up in Spring Wood in the
sunshine at Whalley.
I felt good, but as this goes on, there would no doubt be worse days until I
can learn to cope better.
Most nights between the 7th & the 12th were fine. I was getting up less, as I reduced the liquid intake, but the flow never failed. Sometime it was OK but most times nothing more than slow to start & I had to go a little & often. I could cope with that. Unfortunately there is an element of self kidding. I wanted to believe that its all going to be fine & kidded myself that a “little & often” is normal peeing because I'm an old man. Nowadays, no one is old & I felt like a 50 year old who was a bit sick!
On the 12th. May it was the next biopsy. I went through all the same procedure. They tested my water and the leucocytes showed up so the biopsy couldn't be done AGAIN! I found it very hard to cope with! I never saw the same doctor twice and although everyone was very nice & understanding, no progress was made. I also realised that I NEEDED this biopsy to go forward & get the right treatment & I feared that it would go on for ever. I got seven days of antibiotics to clear up whatever it was, told to drink plenty of fluids to flush it out and await a new appointment with Mr. Javle.
More trouble
By the14th. May I was going back into my 2nd retention!
By 7 or 8am I was in full retention. I tried NHS direct. Nice people but
I needed a locum to put a catheter in. I feared I couldn't wait and sure enough,
by 9:30 no one had arrived, so I headed back to A&E at Chorley.
 Future
advice to you all .. if you go into retention, do not hang about wondering
if it will fix itself... get yourself to A&E sharpish. Its coming! Nothing will
change, & nothing will stop it.
Future
advice to you all .. if you go into retention, do not hang about wondering
if it will fix itself... get yourself to A&E sharpish. Its coming! Nothing will
change, & nothing will stop it.
They let me in very quickly as my records showed I was having the same problem,
but there were no doctors free. By 10:40am I was in a LOT of pain. Finally I was
seen. The doctor was a bit rough & it hurt, but the relief, when it began to
flow, was wonderful. I began my love hate relationship with catheters. I
needed them but they remained hateful objects I had to have!
Hours passed by, loads of question, tests etc., then up to the medical
assessment at Chorley & later on to a ward. It was 3.30 am by the time I was in
a bed.
15th. May...The first thing was a doctor saying I was being transported to
The Royal at Preston. By 10am I was on my way. There was a flurry of activity
around me but I got to see a Doctor. One very pretty Indian Doctor was very good
& understanding, but she wanted to give me the finger up the jacksie test! I think she
was on a learning spree & wanted a good big one to add to her experience! She
really did root around as well, very uncomfortable & very prolonged!!!! Its no
wonder the haemorrhoids never seem to get better with Prostate problems.
The second doctor seemed to be very clear about what would happen. I would be sent home
with the catheter in place & then wait until the next biopsy was arranged. They fitted
a tap on the catheter so that I could stand to pee normally & just open it when I felt the
need. (Often!) It was more discrete & easy to use, so easy you could forget to
close it properly, which I did, several times! VERY embarrassing!
On the ward they were VERY busy, with not enough staff & I didn't get to leave till 4:50. The
staff are superb but they do seem to be overwhelmed at times.
Home again, home again Jiggety Jog!
Once home
I had my first proper shower in ages. I found it was better using underpants to
hold the Catheter more securely. Boxer shorts have no support at all.
Unfortunately, my second pee at home appeared to have blood in it. Maybe this was
the result of my first foray in the upright world instead of staying laying stationary
all day. I rang the lovely Nicola on Ward 10 & she said it was normal, just drink
plenty & keep on eye on it.
On my first full day back home, I had a brilliant sleep. Asleep by 21:30 and slept
through until 7:45, it was heaven. I think you just collapse with the stress of it all!.
At night I had to attach a night bag, it worked well. It was full at 1500 (whatever they are called).
There was no sign of
blood at, all but I needed to be careful with the tubes. Its very easy to pull,
tangle or spill those damn tubes!
I tried behaving “normally”. Walked round to my sons & back, sat around watching
F1, bit of washing & ironing, made tea. It felt worse than it really was. There is
usually an irritant around the head of the penis, the catheter always seemed to
be in the way & in the beginning your so conscious its there. Once it was lightly supported in “Y front”
type undies, it is fine. I think the fear of it
going wrong is worse than anything that actually happens.
All this & we aren't even tackling the cancer yet! I got a nice district nurse who checked me out at home & was as helpful as possible.
I struggled along until May 24th. with the catheter irritating, uncomfortable to sit down, especially with small haemorrhoids I got after all the after examinations. Still it worked well, if anti social & restricting. There was still an urge to go most of the time and slight pain at the end of urinating. I'd been drinking lots, lemon tea, fruit juice, cranberry juice & small beers.
 I had my appointment to see Mr Javle. He had no idea about the retention
problems & that I had a catheter in.
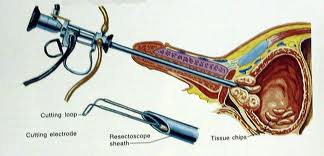
He was very decisive. I was to go in for pre op assessment clinic at 11:15 that
day at
Preston Royal. I had all the tests, MRSA, ECG. blood, urine & answered a LOT
of questions. I was then back in on Wednesday at 9am (it was to be his last op of the
day) to ream out the prostate to make it all work. (called a TURP a Transurethral
Resection of the Prostate). The biopsy would be done at the same time and I
would probably be back home
over the weekend.
I had my appointment to see Mr Javle. He had no idea about the retention
problems & that I had a catheter in.
He was very decisive. I was to go in for pre op assessment clinic at 11:15 that
day at
Preston Royal. I had all the tests, MRSA, ECG. blood, urine & answered a LOT
of questions. I was then back in on Wednesday at 9am (it was to be his last op of the
day) to ream out the prostate to make it all work. (called a TURP a Transurethral
Resection of the Prostate). The biopsy would be done at the same time and I
would probably be back home
over the weekend.
I slept on & off the night before the op. The catheter was still uncomfortable &
I felt the need to wee
constantly. The bag held 900, and it was a perfect straw colour.
25th. May was the day of the TURP.
Operation Willie.
I arrived at 8:45. I was due to go down for my op about 1:30 at the earliest. I
could have gone in earlier, but due to a slight mix up about
only drinking & taking no food, I was delayed. I
had drunk some pineapple juice that morning & that is considered food, so I
couldn't go in
until after 1:30 after all. It was hours of waiting, form filling by student
nurses, gas passers assistants and a staff nurse, plus an inspection by a
doctor. It was 4 before I was called down to theatre admissions. Of course I
told people on my mobile that I was going down, but
I just went into
another waiting area where I was removed from my mobile & I could tell people nothing! Once it was time
to go, I had to walk to theatre … it seemed miles
away and was on another floor!
I had requested a general anaesthetic, but I could tell they were going to do it their way & its just PC
to say I had a choice. I'm sure you'd have to fight very hard to get anything
other than what they say.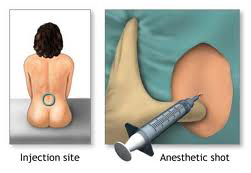
It was a bit of a tragic comedy. This frightened old man was trying to
cooperate with this very nice anaesthetist gas passer who was Hungarian, & as I am a
bit of a deaf old git, I was having her messages translated into Lancashire English by another
nurse in front of me. You get two needles, one for the local area & the other
for a deep freezing epidural. Not the
most pleasant of experiences but it had to be done. She said she would provide a shot of “I-don't-give-a-shit-whats-happening juice” & I sailed through. Your bum warms up, you go numb &
then you can't feel or move a thing. The only thing I felt was the bed moving.
Mr Javle
must have gone for it big time!
I was taken to the recovery area & I felt great, no pain & it was all over with.
Then it was back to ward 15
& I felt fine until around 10pm & then I started to feel the pain. 10pm - until
3am was the worst. I was on night shift with Mick, a huge kindly nurse who got me
through it with drugs & painkillers, still hurting but the edge was taken
off the pain. The catheter was huge as it flushed the bladder and drained it at
the same time. There was
a lovely student nurse called Amy Hall who helped me so much with bed baths,
sheet changing & keeping me comfortable all the time. She will make a great
nurse!
You do learn after a while not to name someone as better than another. You see
all of the staff continually doing their best. You witness kindnesses to old
confused men. You see them clean up stuff, time after time, that you don't even
want to think about, & you know they seem to cope with too much and with too few
people.
Given they have a few spare minutes in the day, you can hear them have a laugh
with people.
The way they manage to prioritise, it must be a skill they just learn over time
& with advice from the senior staff.
The other thing you see, that is blazingly obvious, is that this is the united nations
running the NHS. Every country, accent, creed & colour are here. It is wonderful
to witness.
On the 2nd day of the TURP there's lots of blood & debris. Sometime its clears
but not for long. Lots of Obs. BP, pulse, temperature etc. It ended up that my temperature was going
to be my nightmare, it was never stable.
27th. May was the 3rd day. There's lots of blood & debris still & at one time I thought the catheter needed washing out. I could feel the resistance against passing water. Normally, urine just flows & you're not aware of it, but then I started to feel you need to but couldn't pass it. Having it washed out made a difference & we were back on track again. All the antibiotics were via a cannula in the back of the hand. I lost count of the amount I took but it seemed never ending.
On the 4th day the water suddenly began to flow clearer! The blood was still there but no where near as bad. This prompted doc to say we could have the catheter out if we kept our temperature down. This went on for days!!! At one o'clock 2 consultants turned up with 7 other doctors in tow! Poor devils, I hope its worth it for them. This is where it became apparent that Sunday was the day for the TWOC. (trail without catheter).
I had trouble with the cannula on the back of my hand at about 4pm & it had to be replaced. This always varied from no pain what so ever to DAMN painful! I also pulled my back out moving around and it hurt a lot. The beds are wonderful but hours of laying there propped up, moving very little, sweating & irritated soon gives you other problems.
It took until the 7th day after the TURP to get my temperature stable! Taking it out about noon was damn painful! I was very sore afterwards and took paracetamol. Weeing was painful to start & stung like hell early on. I passed water every hour & it gradually became a little easier. Presumably the large catheter had damaged the shaft of the penis. The extra bad news was the nurse scanned the bladder & it was retaining 230cl. Far too much to be released ... so it was another night in hospital & then check again tomorrow. The even worse bad news was, if I was still retaining urine, then the catheter had to go back in. A big dread, I was very tender & didn't want to even consider the idea. During the long night I was up about every two hours to pass water. The penile shaft was very tender & sitting down was uncomfortable.
The next day, moving very slowly, I actually managed to missed the doctors round. They don't come back, they just told the staff nurse, Joe, their news. Luckily, I asked him & he told me that I was clear to go IF my bladder scan showed it was empty enough. It was 11am that I got the scan and it seemed an agonising wait to find out if it was clear. Boy was I a happy man with the good news that I had passed! Unbelievably, against all previous practise, I was downstairs in the discharge lounge within 30 minutes. That had never happened here before that I could see!
Now for the really bad news
 It
was
a bit of a shock to see how much weight I'd lost and how knackered I was doing the
simplest things. Then things just got worse & worse. With a bad back, problems
with sleeping, exhaustion, and trying to do too much, by the 7th day back home it
was obvious I was starting to have trouble peeing again. My doctor put it down to another water infection.
Back on to antibiotic Frank! I was passing
water in very difficult short bursts. The haemorrhoids were less painful & would
recede better, if I could stop straining every time I went to the toilet.
It
was
a bit of a shock to see how much weight I'd lost and how knackered I was doing the
simplest things. Then things just got worse & worse. With a bad back, problems
with sleeping, exhaustion, and trying to do too much, by the 7th day back home it
was obvious I was starting to have trouble peeing again. My doctor put it down to another water infection.
Back on to antibiotic Frank! I was passing
water in very difficult short bursts. The haemorrhoids were less painful & would
recede better, if I could stop straining every time I went to the toilet.
I had a dreadful night, everything stopped working and I was passing minute amounts of water all through the night. I was so close to going to A&E for yet another catheter, but you'll notice, that with all the experience I now should have, I DIDN'T go to A&E & I paid for it!
By the 8th. full day home, I was kidding myself that at least my water flowed. (Note to self: Not successfully Frank. An egg cup full at a time is crap & how much more do you need to know you're in trouble!)
By the 10th day I was feeling sick, my stomach was very tender & still I did nothing except see my doctor. I honestly think I didn't give him the right information. I pretended I was just feeling rough. I just wanted a magic draught to make me feel better and I dreaded the thought that it was not getting better & I was
going to end up with the dreaded catheter again.
By the 12th day I got up, showered etc but no bowel movement just lots of wind.
I had some pineapple juice & immediately threw it up. Feeling very weak & shaky,
I didn't seem to be able to eat very much at all. I had to see Dr Ahmad at his
morning surgery. He decided to admit me! I looked such a bloody wreck!
One of the major problems seemed to be self kidding. I continually denied the
symptoms & just thought I'm was off colour or needed a couple of
paracetamol's.
So it really is cancer
I arrived at Ward 10 surgical assessment at about 11:45. The problem here appeared to be
lack of staff & doctors as it was all go, assessing people constantly. It
was all
waiting & waiting. Tests like obs, blood & urine were taken with hours of waiting
in between. I was finally given antibiotics & allocated a bed in
the men's general assessment ward.
It took ages of course but the the doctors told me it was a catheter again! This
was where stupidity reigned supreme! I didn't want another catheter did I? Despite
a distended stomach, not passing any water for ages and in pain, I was still not listening to
what the doctor was advising! He told me that retention could lead to real
kidney damage.
Sometimes, when you're ill, you shouldn't even be allowed the vote!
It was bloody awful receiving the catheter. Painful & bloody. It was almost
impossible to move & get dressed again. I put the pain down to the damage
from the TURP and all those
catheters, so I got painkillers to help. Trying to sleep was hell, too much
noise, too many people in pain & needing help. Anyway, that night, 15/6/10, I
thought the painkillers had worked & I was resting better. For some reason, I
thought I better check for leakages as it felt very messy & wet … there, lying
by me was the catheter! It had come out (this is impossible of course!) Blaming
a faulty one, they needed to get a doctor at 2am to replace it. It was 6am
before she turned up & it was the same lady who, I think, had not done it right in
the first place! No staff, no available doctors for hours & its all just a
horrible nightmare! Anyway this time it was fine. Not without pain but working &
secure. A catheter properly fitted has a balloon that is inflated inside the
bladder, preventing waking up with the catheter by your side.
I felt continuously sick & queasy. I was drinking plenty and passing loads of
urine but eating nothing. I hadn't opened my bowels for a few days and the piles
were still irritating. It was not a pleasant time at all. At 18:30 I was allocated a bed
in bay 6 (don't go there, its like an oven & the fans just move hot air around
LOL), but still had the primitive manual bed that requires a nurse to adjust it
as it came from the assessment ward. (Hello, there aren't any spare
nurses to do stuff like that. Of course asking makes you completely guilt
ridden.) Just getting it adjusted meant ringing for a nurse. They are saints
most of the time. Trying to do too much with too few staff. I hated calling
them away from much more urgent cases than altering a bed!
The nights are hell. Asleep at 10:30 & wide awake by 1am. I just laid there
wide awake & there were a 120 minutes in each hour! I was wide awake all the time &
it was hot & sticky. Hospitals are noisy & there were bells going off constantly. It
was a looooong night.
At long last, a consultant confirmed the problem is definitely cancer. It's strange to have all this illness without actually having a definite prognosis. They seemed very vague about why it was proving so difficult to sort out. He just kept saying he wanted me on Ward 15 (urology) to do more tests. He told me that they were to have a meeting about my case on Friday. I was feeling better, in less pain & coping OK, but it all seemed so very indecisive.
 On
the 17th the gang of doctors (well the consultant actually. All the others just
nodded sagely!) said they needed chest, belly & groin scans but no date or time
was fixed. Just after that I was told that Ward 15 was still packed and no
was bed
available. I was called down for a chest X-ray and by 16:00 I finally got a bed
on Ward 15 ... good bye stifling heat and on to continuing not to sleep, &
painkillers giving me weird dreams.
On
the 17th the gang of doctors (well the consultant actually. All the others just
nodded sagely!) said they needed chest, belly & groin scans but no date or time
was fixed. Just after that I was told that Ward 15 was still packed and no
was bed
available. I was called down for a chest X-ray and by 16:00 I finally got a bed
on Ward 15 ... good bye stifling heat and on to continuing not to sleep, &
painkillers giving me weird dreams.
A poor soul with dementia on the ward, and getting less sleep, would be
enough of a problem, but now I had a sensation I was starving all the time! I
only seemed to be eating in tiny amounts as it rests on my stomach like lead.
Maybe it was just not moving around enough. On the 18th the doctors told me that they needed MRI & CT scans, but nothing was booked. That
night I couldn't sleep at all, but they couldn't find a doctor in the hospital
to prescribe a sleeping pill even though its a major hospital!!!!
On the rounds the next day, the doctors were claiming that my cancer was so
unusual that at the next Friday meeting, the whole of the northern hospitals were to
discuss my case. They wanted to put me on a long term catheter, but as my
temperature was fluctuating a lot it stopped them doing this. Instead, they put me on a leg
bag. For the nurses it was a pain to use, as it needed to be emptied often,
but it was be better for my mobility. Unfortunately, when it was full, it felt
like walking with a wet brick swinging around your ankle!
By the 20th I was having hot sweats & seemed to be lying in wet sheets too
often. By the 21st I had had the catheter springing a leak & my temperature was
going mad. I would fine & it would be 38 degrees (too high), another time I was wet
through with sweat & it was normal!
I had changed over to a long term catheter on the same day. It was painful to get the big old
one out and the new thin one was leaky & bloody to start with. I knew they
were
essential but my god how I hated them!
Despite taking a sleeping pill I woke up at 2:30 on the night of the 21st. The
nights were so long & boring. I played the music I have loaded on my mobile phone
(a god send) & sometimes I drifted off, but it was all an irritating nuisance to put up
with. The
catheter took a bit of
bedding in. That was another constantly irritating thing to cope with but it worked
well. I just hope I was not too much of a problem for the staff!
By accident I saw Mr Javle! (even after the operation he had never actually
called in to check on me). He said it was a very aggressive cancer (I didn't
quite twig what that meant when he told me) & difficult to deal with. The
results of the scans that were taken would be at the meeting & they could then decide the
course of treatment. He was thinking of another op because I was a fit
man!!!!!
The 23 June 2010 was a life changing day! It was the day for bad news!
Dr Omi Parikh, who was to be my oncologist, turned up at my bedside during visiting hours without warning. Now Omi is a very plain speaking lady. It suited me, but I can imagine it would cure constipation at a stroke with some patients. She made it clear that the cancer is extremely aggressive. She told me that it is called small cell cancer and that it is as bad as lung cancer. It can spread everywhere in your body. The treatment was to be chemotherapy followed by radiotherapy. The only saving grace was that aggressive cancers are easier to treat than the others. She said it would definitely come back. Her initial thoughts were that I had about 6 months to live! She explained that only 3% of prostate cancers are like this. Trust me to get the rare dangerous one!
No wonder I had been having all these problems. With hindsight, the TURP
seemed to have released the cancer & it spread all over my body.
Early on the night of the 24th the bag was full of blood again over night.
That day I had a radio active injection at 10:30 prior to the bone scan and I was on the
nuclear scanning machine by 1:30. It was a very long & slow procedure, but easy
enough, without any pain or discomfort.
On the 25th, at doctors rounds, they said one of them would come back & report
to me after the meeting & advise what the plan of action was to be. I went for a
CT scan (as machine wasn't working yesterday). It was similar to the previous scan,
but iodine was injected instead of the radio active stuff & it was a lot quicker.
All the doctors seemed to have no idea about the cancer side. I guess urology is
their bag and the cancer, that was Omi's speciality, is not in their field of expertise.
A consultant, Mr Jagnathan, looked on the scans or the results on the ward computer
& said there was a bit of a shadow on my lung. Its amazing, the moment someone
says that, your chest goes instantly tight!
They then got me to do a 24 hours urine collection to check my kidney function. I started the collection at 7am on the 27th. That meant home tomorrow. By 7am the next day, it was all done. I got the notice that I could leave, so Andy, my son, arranged to pick me up around 12, but the admin side was so slow (especially pharmacy!) it was nearer 5 by the time we left. It was good to leave there after so long. No matter how wonderful the staff are, you just need to get away. You just can't do it quickly.
Chemo starts here.
I was back in my own bed on the 29th and it was SO comfortable. A humid night
didn't help with sleeping but it was great to be back in familiar surrounding.
On the first night there was 800 in the bag, all blood & debris. It didn't seem
to be clearing up at all quickly, even through I was drinking water like mad.
I was very weary & moving very slowly. I did too much first thing & had to lie
down! Being in hospital for three weeks weakens a soul LOL
I tried to be as normal as possible over the next few days but it wasn't a
lot of fun.
It was confirmed by phone by the oncology department that I had an appointment
for 9:30 on the Friday. So a new part of this adventure started then.
My meeting with Dr. Parikh made it all very clear. The cancer had spread to the bones, lungs & pelvic area. It is very aggressive, not curable,
& they can only give palliative treatment. They gave me a list of things that
can go wrong that seemed endless. The main problem in my mind would be
impotence. Men find it all very difficult & I'm no exception. (I had to sign a
form to say I understood
all this!!!!). The Chemo sessions were to be every three weeks, the first one being on Tuesday
at 9:30.
So much for it being a simple prostate cancer!
The days & nights before my first chemo were a series of bags full of blood &
debris, feeling shattered, loose bowels & sleepless nights. I even tried
sleeping pills, but they only lasted for 3 hours & I ended up feeling like crap!
 On
the day of the first Chemo, I arrived on time, but I was amazed to find the
procedure took SEVEN hours!
On
the day of the first Chemo, I arrived on time, but I was amazed to find the
procedure took SEVEN hours!
My first nurse was Claire. She was fine, very clear, straight forward & kind.
There was lots
of explaining & I was given my paperwork & advised what MAY happen. (This list
can be VERY long!).
First it was a cannula in the back of the hand (doing this got harder & more
painful as the time passed). The first thing injected in made my bum tingle A
LOT, then it was a liquid to hydrate my kidneys. This took 2 hours. This was followed
by one hour of chemo. Next came a wash out of the tubes and then even more hydration & then
another two hours session of chemo. Apart from putting in the cannula,
it was all utterly painless & completely
boring. Only the tingling stuff gave me any sense of feeling, otherwise there
was no sensation at all.
The machine that dispensed the fluids can be ultra sensitive to movement & could easily just stop working. The stiller I sat, the better it was!
At the end of the session, I left with three days supply of anti sickness, chemo and steroid tablets, and an injection for boosting my immune system. After Chemotherapy, the white blood cells are very low, leaving you open to infection.
The first day after the treatment, the chemo unit rang to ask if I was OK. It
was
all very comforting to think they cared.
I got out there, and continued to try to behave normally. I coped very well with no sign of
any ill feeling, just taking it one step at a time.
On Friday the 9th. the district nurse turned up & gave me the injection I had brought from the unit and kept in the fridge (its stings!). All was well with me. There was a slight feeling of sickness but it was nothing to worry about.
On the 10th there was 1200 clear pee in the bag. I went out all day & had a great time, but the night turned weird! After a long time of not sleeping I started to feel like I was collapsing about 9 pm. I had to give in at about 10 pm & then spent the night dreaming of feeling sick. The next day was spent feeling queasy & tired with a tight chest, but nothing too bad. I just keep resting as I hadn't a lot of energy at all.
Back to hospital.
On the day of the 12th I sensed something was wrong. My temperature was banging against the magic number of 38 degrees. Once this is reached, you have to report back to the hospital as the white cells are so low that an infection risk becomes a dangerous possibility. By 5:20am, it was at 38.2. After phoning the hospital I was instructed to report to the clinical assessment unit straight away.
This is where the theory & practicality bang head to head. All the tests were done, full obs including a blood test, but a surplus of ill people and lack of staff, doctors & beds meant a 12 hour wait until I was in bed & getting treatment. I think it was just too long. It resulted in a hospital stay of 15 days because I had a VERY bad chest infection.
I was very ill, pumped full of antibiotics & it was a rough time for sure. I was on Ward 24 which was the chest specialist ward. We had two very confused men in with us. The nights were very difficult for all of us. Lots of shouting & arguing with the nurses. Just how they coped was wonderful to see. They were such a credit to their profession. No wonder they are called Angels.
Omi arrived about the 15th & quickly got things sorted. She was concerned at the delay in my admission & thought the danger of cross infection on the ward was too high, so I was allocated a single bed side ward. It was great for my nights sleep, lonely & cut off from the daily interest of the ward happenings .... but oh so peaceful!
I got weighed sometime during the week & was 74 kg in my hospital PJs! (that is well under 12 stone ... I had certainly lost a lot of weight).
The worst part of the treatment was an antibiotic called Clarithromycin. Real bitch stuff! Its like taking Domestos or Jeys fluid in the veins. LOL. It was ages before I found out that it could be given orally as a pill. OK it maybe less effective but I'd rather take longer & take the funny taste it gave me in my mouth but at least it was not painful. (of course, this COULD have killed me in the meantime) It was no fun to be in bed with a burning cannula fitted to your left hand & your catheter bag on the floor on the right hand side. Its a great way to pin you down! Not that the staff weren't wonderfully helpful & considerate. There just wasn't enough of them & they had no spare time at all.
The food was very good, the beds were cheerfully changed every day & the cleaners were omni-present keeping the place safe for us all. Although I think I was so +ill because of the delay in admission, what can you do if the NHS doesn't employ enough staff & has too few beds?
I was finally released as fit on the 21st.
Made it to my 72nd Birthday
The first signs of the chemo showed as I showered at home & huge lumps of hair blocked the plug hole!!!!
Once I reported back to Omi & took my second scheduled dose of Chemo, she cut it down by 25% & I had very few further illness problems. I had the sessions three weeks apart on a Tuesday. By Saturday I usually had a sore throat (never really bad). I was SO glad to be peeing freely, even if it meant the dreaded catheter, & I was not really ill as I took the treatment. The only other symptom was very erratic bowel movements. Despite everything I was one happy man! I made sure that I lived life as normally as possible, taking regular breaks away from home.
Half way through the chemo sessions, there was a scan to check progress & the result was excellent. Great progress had been made. The size of my prostate had shrunk so much that the report said I'd had my prostate removed, which of course I hadn't. A scan at the end of the Chemo session was even better. Although it remains extensively in my bones, it had cleared from my lungs & was much smaller in the pelvic area.
Free Willie!
It was November before I had the long term catheter removed. When they told
me it was to go, I just burst into tears. The catheter may save you but never a
day went past without me cursing it! After such a long time (about four months)
I was truly frightened it wouldn't work. The thought of having this bloody thing
attached for ever was fearful to me. Of course, now I can say it went without a
hitch. It came out easily, there were quite a few "accidents" as I learned to
control my bladder again. I used pads to begin with, to soak up leaks, much
longer than necessary, but that was me not coping more than there being
continuous problems like willies that could drip at the most inconvenient moments. It
would not
behave in a dignified manner if you laughed too loud, bent down to tie up a shoe
or cough! Remember the saying gentlemen know so well? "No matter how you stand &
shake your peg, the last two drops run down your leg" Well you should try
prostate cancer, its a LOT worse! Unless you have experienced the problem of
retention, catheters & all that goes with it, its hard to imagine what a
wonderful thing it is to pee freely, on cue, & without embarrassing
yourself! As a friend of mine says, "It's heaven with the gates shut"
So Omi decided, even though we didn't know how many more Christmases I would see, that I was doing really well & the treatment should be expanded. If this is a terminal illness, its not started off badly. I would hate a cancer that caused me pain (my religion won't allow it ... I'm a devout coward) & I still consider myself to be very lucky. I'm still here after 9 months & living life to the full. Every laugh, love & sunset seem a huge bonus. Having cancer helps you see what is important in life.
More treatment into 2011.
So the treatment carried on. Every 12 weeks I report to Doctor Ahmad & he
gives me a hormone injection in my stomach. Then in the New Year, I began a
series of radiotherapy sessions. First of all there was a machine to set up all
my measurement. There was a lot of
explaining & to my surprise, I was given four tiny tattoos, so that the body could be
lined up correctly each time. They did ask if I would mind permanently marking
my skin ... of course, I never guessed they would give me tattoo marks! The sessions
were every day, except weekends, for ten days. It
 took longer to undress & dress again, than it took to have the treatment.
There was a lot of accurate measuring, especially on the first session. Two
operators checked the figures before going ahead. I had four shots each time.
It was all utterly painless, very quick & the only side effect I got, could be fixed with the occasional
Imodium tablet.
took longer to undress & dress again, than it took to have the treatment.
There was a lot of accurate measuring, especially on the first session. Two
operators checked the figures before going ahead. I had four shots each time.
It was all utterly painless, very quick & the only side effect I got, could be fixed with the occasional
Imodium tablet.
Joy of joys, by the end of the radiotherapy even my hair had begun to grow back! Mind you, it's turning out to be curly/wavy & a lot thicker. In fact, it seems to be covering my bald spot! At the back, before my first cut, it looked like a Marcel Wave. (only the older people will comprehend what one of those is!).
Since all the treatment started last May, the only strange thing that doesn't seem directly connected, is aching legs. At the moment we're working on it, to see if its the cancer in the bones that's causing it, or Simvastatin I take for cholesterol. Some time later, I managed to pull what seemed to be a muscle under my shoulder blade. Doctor Ahmad thinks that it could be connected to the treatment & I will have to follow it up with Omi.
Cancer strikes back!
At the meeting in early March, Omi was in no doubt that the aching legs
(which were gradually getting easier) was not the cancer & what felt like pulled muscle
was actually the cancer that was now in my bones. A CT scan, more radiotherapy & some treatment for
strengthening bones was in order.
The pain I felt was in the centre of my back to begin with & seemed to be affecting the muscles around it. (I often seemed to get more pain relief from Ibuprofen than the Co-codamol I got from Dr. Ahmad on prescription.) Just before my initial assessment for the next treatment of Radiotherapy, a second area to the right hand side of my bum appeared to be painful too. Omi & her staff measured me up for both areas, took their readings & organized a daily session of radiotherapy beginning on the 21st. March. This was a week before a planned break in Somerset. It was very different from my first session. Originally, I had four brief shots lasting between 8 & 12 seconds. This time is was two shots of around a minute each! The nurses warned me that it would get worse before it got better & they were so right. The pain is never unbearable just very uncomfortable. Doing too much would wear me out. I was always anxious to see everything & do everything in case it was my last chance. The pain was always at its worse after long periods of sitting still, staying in one place too long, or after a nights sleep. The feeling never left me that it was the muscles sending the signals that the cancer was showing up through them.
On the 4th of April I had another CT scan. The scans are never a bother at all but it is obvious that putting needles in for any reason (this time is was a tracer dye that helped show up the scan results or at other time a blood test) the staff had more & more difficulty finding veins. It took four insertions before it was working correctly. They were more painful than the cancer!
On that Friday I had my meeting with Omi, & although I was feeling as good as I ever had been, she had to tell me the cancer had come back in my lymph nodes & I had to go back on chemo therapy. The bone strengthening was delayed & I am just waiting for my dates to start it all.
Oh well, no one promised it would be easy! Back to baldness & with luck just an occasional Imodium. Lets hope I don't get ill again. I have another holiday planned in Cornwall. I don't want that mucking up!
 Had the chemo on 28th, and as usual it was a doddle. Laura, my nurse,
even found a vein easily without much pain at all. As before, there was lots
of discussion about what COULD happen but you just have to wait & see. Most
commonly, chemotherapy acts by killing cells that divide rapidly, one of the
main properties of most cancer cells. This means that it also harms cells
that divide rapidly under normal circumstances: cells in the bone marrow,
digestive tract & hair follicles. This results in the most common side
effects of chemotherapy : decreased production of blood cells, hence the
suppression of the immune system, inflammation of the lining of the
digestive tract, and hair loss. The last time I was very ill with an
infection, certainly lost my hair & usually had a mild sore throat. I also
needed to use an occasional Imodium but nothing serious.
Had the chemo on 28th, and as usual it was a doddle. Laura, my nurse,
even found a vein easily without much pain at all. As before, there was lots
of discussion about what COULD happen but you just have to wait & see. Most
commonly, chemotherapy acts by killing cells that divide rapidly, one of the
main properties of most cancer cells. This means that it also harms cells
that divide rapidly under normal circumstances: cells in the bone marrow,
digestive tract & hair follicles. This results in the most common side
effects of chemotherapy : decreased production of blood cells, hence the
suppression of the immune system, inflammation of the lining of the
digestive tract, and hair loss. The last time I was very ill with an
infection, certainly lost my hair & usually had a mild sore throat. I also
needed to use an occasional Imodium but nothing serious.
This time the CAV treatment (commonly used for lung cancer I understand) only took just over an hour. That makes it so much easier. There was no sitting still for seven hours, trying not to disturb the pump that is filling you up with chemo. Seven hours can feel like the whole day!
My pee has turned pink (I was warned it would) but apart from that its far too early to tell. We set off on holiday tomorrow, breaking the journey in Bromsgrove. I am taking a mountain of pills, anti sickness, steroids, (Oh my life, that makes you eat & not sleep) & an injection to be given tomorrow to boost my white blood cells. Luckily, Cynthia's cousin Penny is a retired nurse, so I'll be getting it from an expert!
Taking a break
So off we go, trying to have a lovely holiday without picking up an infection. Apart from a mask & snorkel, a full body condom, marigolds & plastic bags over my feet, there is little you can do apart from being sensible. Avoid crowds, follow the advice in the chemo booklet, wash your hands a lot & use anti-bacterial gel!
The holiday was excellent. The only thing that happened was that I either ran out of puff a lot more, or I tried to do too much on the holiday. There are no flat bits in Cornwall, so huffing & puffing came with the deal. There was no sign of any temperature or illness & therefore no need to go to an A&E unit at all. A slight by product of cancer is that every twitch, pain or grumbling tum makes you think something is wrong. I'm sure, under normal circumstances, I would ignore everything & just carry on.
I reported to Omi's registrar on Friday the 13th! I had nothing to tell
him, except I was just a
happy man progressing well after my first dose. The next chemotherapy treatment is due on
Thursday. As my blood's white cells should be on the recovery phase, I'm
expecting no problems. We are enhancing the session with a dose of bone
strengthening. To make sure I was ready for this, (after a few sessions, it can make dental
treatment a hospital job apparently) I had a check up at the dentist & he
told me I needed no work doing at all & that my teeth were good for another ten years! (I should be so lucky!).
progressing well after my first dose. The next chemotherapy treatment is due on
Thursday. As my blood's white cells should be on the recovery phase, I'm
expecting no problems. We are enhancing the session with a dose of bone
strengthening. To make sure I was ready for this, (after a few sessions, it can make dental
treatment a hospital job apparently) I had a check up at the dentist & he
told me I needed no work doing at all & that my teeth were good for another ten years! (I should be so lucky!).
By Saturday the 14th. my hair had started to fall out in lumps! It seemed to happen much quicker than my first loss & damn suddenly! Oh dear, yet another close crop by my son tomorrow morning!!!!
On with the chemo
I reported for my second chemo & first bone strengthening treatment together on 19th May. It took a little longer but no real problems, apart from a timing mix up & the usual trouble finding a vein. Taking Chemotherapy is completely painless, it's just taking care afterwards that can be the tricky bit. In the next two days it was more anti-sickness and steroid pills plus an injection to be given after 24 hours. Then a minor miracle occurred! Cynthia, who used to faint with monotonous regularity at just the sight of a needle, (in fact she once managed to fracture her skull having a very minor injection), is now my injection nurse & manages to, not only give it, but I don't faint either!
This running out of puff in the first week is a major occurrence I can't ignore! My body feels like its wearing a lead night shirt with a tight chest & slight aching over most of it. Just trying any kind of exertion drags you to a stand still. Going to bed and sleeping for 12 hours seems common. I have to take afternoon naps, well actually, its more like a short course in death for an hour! There is also the problem that if you don't try moving, you feel you'll become comatose. The first two days are not quite as bad, as you have steroids but after they run out, you feel like Dickens' Marley must have felt, without the noise the chains make, just the weight!
The appetite is fine but this time there is an uncomfortable acid reflux in the throat, but an occasional Gavison helps here.
There was a suggestion that the bone strengthening would give me a feeling of having flu, but very little has happened & I've avoided any real illness.
During the second week, it was just a slow recovery with minor aches & pains and an occasional bad night, but on the whole, easier than expected.
At the end of the third session it becomes clear that the first week is mainly exhaustion, the second week is mainly tired & flu like (very mild & easily fixed) & the third week is fine if you take your time.
On the 15th of July I have a meeting with Omi to tell me how well/badly I'm doing, if its anything to do with how I feel, it should be good news!
 Back to the good news!
Back to the good news!
By now I was on my fourth session out of six of the chemotherapy before I had my appointment with Omi. As usual the place was full of people either seeing their consultant or have their treatment. Everyone seemed a little delayed, as it was so busy, but they were an amazingly healthy looking bunch. Omi had been most kind & written me a brief letter saying that the scan showed excellent progress. I am sure a consultant oncologist has better things to do than send out letters, a week before I was to see her! Nevertheless, once she walked in the room, I could tell she was surprised to see me looking so well! She constantly reminds me that this is a very aggressive cancer and it just may be my optimistic outlook that is keeping it at bay. I tried to tell her how I feel, but the number of small symptoms I have, made it sound as it I'm having a bad time. Nothing could be further from the truth. The worst thing is my restless legs ... which has nothing to do with the cancer I'm sure. Then there is the utter weariness of that first week, occasional small problems like constipation or the trots for a short time (a pill fixes it very quickly), and also the aching around the second week, which again is soon fixed with a couple of paracetamol.
I continue to live life to the full. Treat every day as a bonus & as I'm not in any real pain, I'm a very happy man. I'm sure it won't stay like this for ever but until it changes for the worse, life is good.
Our dash to see Pat, one last time.
 Pat
had been our best buddy on our website for a long time. She was Cynthia's
friend for ages and was there for Cynthia when I first found out I had
cancer. A wonderfully funny women, full of fight & a heart as big as an ox.
Recently widowed from "Gorgeous George" she tried hard not to let life get
her down. For years, she suffered from COPD (Chronic Obstructive Pulmonary
Disease). It made her constantly breathless & subject to lots of chest
infections but it never seemed to beat her.
Pat
had been our best buddy on our website for a long time. She was Cynthia's
friend for ages and was there for Cynthia when I first found out I had
cancer. A wonderfully funny women, full of fight & a heart as big as an ox.
Recently widowed from "Gorgeous George" she tried hard not to let life get
her down. For years, she suffered from COPD (Chronic Obstructive Pulmonary
Disease). It made her constantly breathless & subject to lots of chest
infections but it never seemed to beat her.
Very recently she was diagnosed with lung cancer. Because of her fragility, they found it hard to treat. Despite this, she seemed to be on a upward curve, life was getting better, she got out more & was looking forward to a holiday with her daughter Sarah & her partner Chris, across on the Welsh coast at Saundersfoot. They took with them her two "doglets" Albert & Freddie ... well they are her very hairy children really!
She was having a wonderful holiday, in fact she told her daughter it was one of the best she'd ever had. At the end of the week she started to suffer some severe stomach pain and was admitted to Haverfordwest Hospital with Gall stones! As if cancer, gall stones & then septicemia were not enough, she was then told that the cancer had spread to her liver.
She battled on, still with her mad sense of humour, so breathless that she made her daily phone calls to us very short & very gradually she became so weak, she stopped responding altogether. We were lucky to have Sarah to keep us up to date.
 Then we got that phone call to tell us it was all drawing to a close & if
we wanted to see her, we should come now. News like that from doctors isn't
given lightly. To be honest, I thought we might not make the 250 miles plus,
in time.
Then we got that phone call to tell us it was all drawing to a close & if
we wanted to see her, we should come now. News like that from doctors isn't
given lightly. To be honest, I thought we might not make the 250 miles plus,
in time.
She appeared unconscious. Just lying there breathing slowly. We hope so much that she knew we were with her but there was no sign. Surrounded by her friends & family, it was all very peaceful & we all tried to stay cheerful for her. Being Pat, she had to have her last laugh. She would occasionally, take a deep sighing breath & then pause long enough for us to panic, and just as we were about to call the nurse ... she'd start breathing normally again! What a girl, game to the last!
Of course for me, it was great to make it in time, lovely to see her at peace & in no pain. Plus I could actually see that palliative care is so good. They kept her out of pain. She was able to say her goodbyes & just gradually slept more & more & then just slipped away about three am on Friday morning the 5th August 2011.
God, we are going to miss all those phone calls we had after we had text her. She never did truly master that bloody awful Sony Ericsson mobile phone. No more posts on our website. No more visits to her flat in Barry, being spoilt rotten & licked to death by the doglets & no lovely shoulder to cry on. We'll miss her so much but she showed me that the end could be very peaceful & I'll be ever grateful to her for that.
Pat was buried with her beloved "Gorgeous George" on a sunny Tuesday, the 16th August 2011. On her coffin was a brass plaque, which included a picture of Freddie & Albert. She was seen off by her family & friends, and although tears were shed, laughter could be heard & smiles seen all around the room at her wake later on ... just the way Pat would have liked it.
What would you like? The good news or the bad news.
 It
was the day after my 73rd birthday & I was due to see Omi Parikh at 11. Of
course, she had that many clients and she was running late as usual. So we hung
around & finally saw one of her registrars, a nice pregnant doctor who was
most pleasant but not as clear as Omi. Luckily, we got to know that Omi
wanted to see me. How nice is that? I know she is busy but she seldom fails
to find time to fit me in. Once again she looked astounded at my good health!
She was delighted but puzzled, and I said I hoped I was not upsetting her
statistics! It took longer to tell her about my progress & how well I felt
than it did
to hear that the news was very mixed.
It
was the day after my 73rd birthday & I was due to see Omi Parikh at 11. Of
course, she had that many clients and she was running late as usual. So we hung
around & finally saw one of her registrars, a nice pregnant doctor who was
most pleasant but not as clear as Omi. Luckily, we got to know that Omi
wanted to see me. How nice is that? I know she is busy but she seldom fails
to find time to fit me in. Once again she looked astounded at my good health!
She was delighted but puzzled, and I said I hoped I was not upsetting her
statistics! It took longer to tell her about my progress & how well I felt
than it did
to hear that the news was very mixed.
The scan report says its still in my bones and that most of my cancer is "stable" (its not gone away or changed). The lymph nodes weren't mentioned (that's what I had the last chemo treatment for) but there is very slight growth in the small cancer spots in my lungs, (which I thought had gone away) and this growth happened while I was having treatment. (Surely that ain't good news?).
The prognosis from Omi was that I should have a rest from treatment but see her in 6 weeks with a view to another scan in 8 weeks or commence further chemotherapy. She has no doubt that it's coming back & this is a balancing act between quality of life & more of the aggressive stuff pumped into me. She even intimated that most terminal patients don't get past two sessions of chemo and we are in new territory on how to go forward.
It's my first time at this terminal cancer thing and it's what she has trained for years to do. I trust her judgment completely.
Despite all, the meeting was fun & full of laughter. I feel well enough to put up with anything they need to give me. In a little while this "3 months to live" will be up to 18 months & I'm buggered if I'll go down without a few laughs & a fight. Anyway, we have four more short breaks booked & why lose the money? Us small aggressive men are like that. LOL.
Looking towards the 3rd. chemo session
 The visit to Omi was as pleasant as ever. We laughed a lot & between that,
& telling me she is off on her holiday to India in a week, we decided it was
to be another scan, more chemo, similar to the first session I had, but
shorter than the 7 hours I hope. Then it was a run round the hospital trying to
re-arrange scan dates, as the one they had planned was on the week of our
next break in Northumberland. Everyone was most obliging & tried to help where possible.
The visit to Omi was as pleasant as ever. We laughed a lot & between that,
& telling me she is off on her holiday to India in a week, we decided it was
to be another scan, more chemo, similar to the first session I had, but
shorter than the 7 hours I hope. Then it was a run round the hospital trying to
re-arrange scan dates, as the one they had planned was on the week of our
next break in Northumberland. Everyone was most obliging & tried to help where possible.
Then it was back in the chair to get more bone strengthening treatment. It's short & painless, apart from getting the cannula in of course. Finding any vein is getting very difficult. The last blood test took three goes ... and these girls do it every day.
The next chemo, combined with the bone strengthening, has been fixed for November the 18th at 10 am. Wonder if that means it's going to be a longer day than I hoped? That will also mean a blood test the day before. Omi has arranged to see me the following week. Oh well, back on the treadmill again! Better get another break in while we can enjoy life to the full!!!!
During the holiday, I felt a pain in my back, probably due to me getting above my station moving a four poster bed (you'd have to read the story!) So I visited Dr. Ahmad & he's put me on a stronger Ibuprofen tablet plus Co-codamol & slowly it's doing the trick until I get to see Omi. I suspect she'll give me another dose of radiotherapy.
18th November & the third cycle of Chemo
 The
treatment has changed a bit after the results of my last blood test. I'm no
longer on bone strengthening, because it is having an adverse effect on my
kidneys, so now it's just two kinds of chemo.
The
treatment has changed a bit after the results of my last blood test. I'm no
longer on bone strengthening, because it is having an adverse effect on my
kidneys, so now it's just two kinds of chemo.
Once again the Angels (it's definitely the right name for nurses) set to
work pumping poison into my body! This time, Sheila started it all off and I
was sorted out by Sarah & Maxine. Poor girls, every time they have to do any procedure at all,
 they are required to don a plastic apron & latex
gloves ... no, not just for their protection but to stop germs from
attacking me. Bless them, they are SO conscientious. They check it's the
right stuff, ask my DOB & address to make sure another OAP hasn't sneaked in
to nick my personal, handmade chemo. God know what will happen if I get
Alzheimer's & I forget Cynthia, & come on my own! I always feel that on my
next visit, a new rule will have come out & they'll have to wear the plastic
apron, the gloves plus a mask & snorkel with a full body condom.
they are required to don a plastic apron & latex
gloves ... no, not just for their protection but to stop germs from
attacking me. Bless them, they are SO conscientious. They check it's the
right stuff, ask my DOB & address to make sure another OAP hasn't sneaked in
to nick my personal, handmade chemo. God know what will happen if I get
Alzheimer's & I forget Cynthia, & come on my own! I always feel that on my
next visit, a new rule will have come out & they'll have to wear the plastic
apron, the gloves plus a mask & snorkel with a full body condom.
As usual, the finding a vein was a game in itself but Sheila found it in the end. The Chemo is no bother. It wasn't ready at the appointed time, so we made a nuisance of ourselves by acting the fool (out of sheer boredom of course). I'm not sure how long it will be before they actually ban me! As Cynthia & I have booked more short breaks, the girls were great at fitting it all around our requirements. What stars they all are!
The next thing is to get over the next two weeks without becoming ill. By the Friday, I was as weak as a kitten again & for the first time, I got a mouth ulcer. It was lots of small problems that accumulated. Sickly stomach, odd aches & pains that come & go. Its nothing that I can pin down, just a rougher feeling than normal. I slept odd afternoons but the constant waking at night is a pain. Lots of needing to pass water & my legs "fizzing". Cut down the coffee & sugar again!!!
Oh well. Onwards & upwards, lets try & kick it to bits & laugh in it's face!
Things go t*ts up again
I saw Omi about 11am on the Friday, she was her usual supportive self, calling me her miracle patient cos I look so well. She prescribed a list of huge bottles & potions to combat the indigestion & mouth ulcers, & although we knew the tumors had grown (we knew they had last time), Omi hoped the chemo would help shrink it back.
I probably did too much & being run down, I got an infection. On the way home I got the car fitted with two tyres & had the brake shoes changed, then on to Ian, my son's home for a hair cut & then a small carvery on the return leg. I wasn't eating much as my stomach was giving me more indigestion & by about 6 o'clock I was shivering as my temperature started to go up.
 I checked it at 7:10pm it was 38.1. By 8 o'clock it was 38.2 ... time to
ring the out of hours number for help (38 degrees is bad!). This time I was
lucky. Damon the ward manager on the Ribblesdale cancer ward had a spare
bed, a bit of a rare occurrence, and by 9:30 I was sitting by the side of bed
17 in bay 4, my home for the next 7 days. There is a fear that you will be
called in & no spare bed can be found, that's what happened last time & it can be very
dangerous.
I checked it at 7:10pm it was 38.1. By 8 o'clock it was 38.2 ... time to
ring the out of hours number for help (38 degrees is bad!). This time I was
lucky. Damon the ward manager on the Ribblesdale cancer ward had a spare
bed, a bit of a rare occurrence, and by 9:30 I was sitting by the side of bed
17 in bay 4, my home for the next 7 days. There is a fear that you will be
called in & no spare bed can be found, that's what happened last time & it can be very
dangerous.
Annoyingly, my temperature was normal by the time they checked my obs. at 10 o'clock!
That night I was to experience the first signs of what a great team they have running Ribblesdale.
Damon is a huge man, reminds you of a very young Desperate Dan, looks like he eats cow pies & can lift the electronic beds with just one hand. He gives out confidence & you know you're in safe hands. My first nurse was Mirela, a slightly mad Romanian who made you smile & just did a great job looking after all the patients. She assured me I wasn't going to get a lot of sleep as I had to have drips for saline, antibiotics & even an ECG during the first few hours. Once you're in there, you realise there isn't a lot wrong with you, that given time, these guys can't fix. They all seem over worked and short handed, but able to cope no matter what is throw at them. I'm sure that in theory, if nothing goes wrong, there are enough staff on duty, but throw in poor old men with dementia that cause all kinds of trouble, cancer that suddenly needs instant attention as people pass out, & other things that you know are happening all over and you realise there aren't enough hands or hours to deal with it all.
With hindsight, I just needed lots of antibiotics and stuff to fix a stomach
that was giving lots of problems with anything I ate or drank, except milk.
The doctors said that whatever was
causing the fever would probably never be known but I had the worse blood
count ever & there was nothing there to fight the infection. I was given lots
of saline because I wasn't taking in enough fluid. The trouble is that by
now my veins were collapsing at an alarming rate because of all the chemo I
was taking. I had to have cannula after cannula fitted as they ceased to
work. Every day blood had to be
taken at least once. I
was like a pin cushion! Apparently there is a thing called a Picc line,
a peripherally inserted central catheter (PICC or PIC line) is a form of intravenous access
that can be used for a prolonged period of time, it stays in the body
permanently. I'm sure I'll end up with one eventually.
The next days were just more of the same, with an occasional change like the chest X-ray I had. Without fail, every shift, yet another excellent nurse covered the ward. Polly was followed by people we knew from the day case unit, Sarah & Jed. Nicer more considerate people you couldn't wish for. Jed looks after his ward like a mother hen. He is so attentive & no matter how busy he is, he seems to find time to make sure you're happy with what has to be done. On nights was a Polish nurse called Bonzenna (bet that's mis-spelt!) she was quietly attentive, tried hard not to disturb anyone but really looked after us all. People like these are such a credit to the NHS.
The only difference this time was the same doctors were to appear regularly. Not like the time I was in Ward 15 when I never seemed to see the same one twice. Only twice were we invaded by consultants with junior doctors in tow. (The most was 10 people round one bed!). This time the doctors were more human, less clinical & seemed genuinely happy to see the progress I made. Only one consultant seemed of the old school, he complained about the noise ... pity happy patients & staff are considered a bad thing!
The other thing that staying in hospital reminds you ... it's run by the united nations! I bet there isn't a country, race or religion not covered by the staff here. It's wonderful to see. Sometimes the accents are hard to understand ... they even had a Scouser & her mate from Thirsk! Oh my God, it was like a female Laurel & Hardy double act!
After a time they had fixed the tummy, got the blood count up and stablised the temperature. To add a bit of muscle to my blood count, they gave me two units of blood & my last antibiotic. What a day that Friday was. They had had several brief power failures, the computers in blood testing were down, so it took a long time to get the results and my demob papers!
You can never be grateful enough to people who keep you alive but they all seemed to know how much I appreciated them as I left. It's just a pity, because of shifts, you can't tell each one personally. All you know is that its a team effort; Right from the ward cleaners, the domestic staff, volunteers, angels & doctors. Its an international effort & I'm still here to prove it works.
The good news is, five days after leaving hospital I managed a few days away with very few problems. The bad news is my hair fell out over three days! LMHO. I wonder if that stands for Laugh My Hair Out?
The meeting with Omi
It's now a week off Christmas & there was snow. Doctors couldn't get in but Omi did! Nevertheless it was a mix up with notes & a long drawn out wait.
She hadn't been informed of my visit to Ribblesdale & was somewhat surprised. Luckily she had already reduced one of my Chemo's because of the effect it was having on my kidneys. She couldn't give me more Radiotherapy as that could have been too toxic. She's planning another scan too to see the progress. So long as I can keep the nagging back pains under control, she hopes that the shrinking of the tumours will help. Of course people don't usually get this far with chemotherapy & I seem to be too stubborn to give in to it.
So it's onward & upward until our next meeting on the 6th Jan 2012.
It's likely to be our last as Omi is on maternity leave soon & I'll have to
change consultants.
 God I'll miss her!
God I'll miss her!
So we make it through to Christmas!
This time the chemo really knocked me out. From about day 5 to day 9 after the treatment I literally gave in & did nothing. I hadn't the choice really. Just showering & dressing wiped the morning out for a while. The pain gradually eased but I had a constant struggle eating & feeling comfortable. Cynthia fought bravely to cope with a cough & cold, trying so hard to stop me getting it. She was awash with antiseptic wipes & used millions of tissues. It looks like I escaped a cold but only time will tell.
Xmas dinner was a joy. I was well enough to enjoy every mouthful. Tomorrow & onwards I hope I have the energy to complete Christmas with family visits & the travelling involved.
The good stuff doesn't last that long.
On Boxing Day we went across to meet all the family & it was just lovely for us to get together. Ian & Bev did so well coping with a family trauma and meeting & feeding over a dozen souls. I was feeling fine but not able to eat anything with spice in it, so Ian's lamb casserole was the hit of the evening for both Cynthia, with her dietary problems, & me.
We were feeling good & on a roll. The next day we travelled down to the Midlands for Christmas with Cynthia's family and had a lovely day. Then after an overnight stop we had breakfast with friends, before meeting up back at our flat, with eldest son Andrew, granddaughter & her partner Mark, to end a really nice Christmas period.
Over the next few days we thought we had done too much because once again the side began to get more & more painful & we automatically put it down to doing too much and sitting in the car for long periods.
Maybe we should point out that if anything goes wrong, like earache, ingrowing toenail or the first signs of leprosy, you immediately blame the cancer (and you're probably right!) but with cancer, where you think the trouble is, is not likely to be where the problem is! In my case it was usually pain on the left hand side just under my rib cage. It was not guaranteed to stay there, but it was a pain, not an ache. It felt like the tumour was resting on somewhere & I could only get relief laying/sitting in certain positions. It got worse as time went on, and, as often happens this was just as we were heading towards a Bank Holiday and my next chemotherapy treatment. . Over New Years Eve & New Years Day (with Chemo treatment due the next day) it was getting close to unbearable.
I couldn't bear to sit in any position. There was relief if I stood upright & I could only sleep flat on my back. This gave me the impression, once again, I was catching the growth on something. By Tuesday 3rd, I was in agony & needed help. Where do you go to get help & advice over the phone? Pauline, Omi's outstanding Secretary!
We were in the ludicrous position of trying to get me across to Preston Hospital, (an hours journey away) to get a blood test & then the Chemotherapy some hours later, with me having to lay flat on my back on the reclined passenger seat, as the pain was on the edge of stopping me being able to doing anything.
Cynthia rang Pauline for advice & to ask if we could see Omi, or her registrar, & to sort something out for when I arrived (IF I could arrive was beginning to seem a possibility!). What a wonderful efficient lady! Although Omi was working in Blackburn all that day, she organised everything within, what seemed, ten minutes. We soon had a return phone call to say that I was expected in the unit and everything was organised.
When the NHS swings into action with people like this, it just happens. EVERYTHING worked & before we knew it, I felt I was in safe hands & heading towards some kind of resolution.
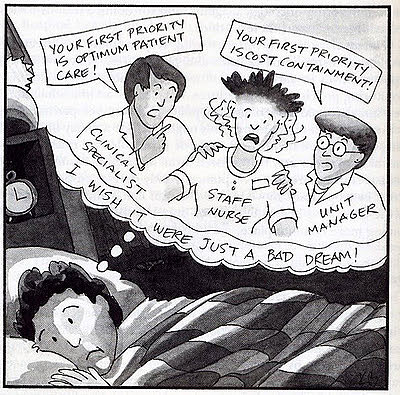 The NHS swing into action!
The NHS swing into action!
I had a bed waiting for me to lie on as I was assessed by Dr. Chen, a lovely lady who was very thorough & had already planned the MRI scan in advance after advice from Omi. I was waiting again to be fitted in available slots but not for long, as had happened in the past. It was all down to Omi, Pauline & the NHS. This is not intended as a set of compliments but just a statement of how it appeared to me. After the scan & its analysis, it was Dr. Chen's task to give us the bad news, which she did well. It appeared to be a compressed vertebra trapping a nerve, that had the potential to take away the use of my legs (that's another thing that can be used to cure constipation very quickly!).
Provisionally I was allocated a bed in Ward 2B, the area next to the high dependency unit, with the prospect of major back surgery. I was so lucky to get a bed and it was in the new extension as well... lots of room around each bed & a cooler ward than usual that was a pleasure to be in. There were just four of us, mainly with poor mobility, & we all needed looking after. We had lovely staff too, Faz & Bev I remember so well. There were many more but with shift work, lots of sleeping with the magic of a small purple pill of Morphine, (my life saver without doubt!) I didn't put down their names.
To put it nicely the first night was interesting! I was put on steroids & morphine, plus tablets to prevent any stomach problems from occurring, daft airline socks to prevent DVT, & laxatives (with the stuff I was taking, it needed a lot too!!!!). I was out like a light to begin with, but then the one o'clock chorus started. There will be no names nor pack drill but it was fun! One of the lads could snore for Great Britain. It ranged from a gentle kitten's purr, thru a lion & tiger mating reluctantly (OK I haven't too much evidence to go on but I have a great imagination.) He seemed to meet his crescendo with an imitation of the last fog horn on the Titanic. Opposite was the most gentle & almost poetic man talking in his sleep. You could hear every syllable, but like all the right notes, but not in the right order, many of the words were pure nonsense. The classic set was a deep sigh, a whispered "Popeye the sailor man", (truly!), a soft paddle to the bathroom & then a mumbled incomprehensive phrase of deep satisfaction afterwards. Unlike many, this was a soft gentle person & there was never a hint of aggression. One of the lads had sleep apnoea & his machine gave out many weird & wonderful support noises. Luckily, Mr. Morphine got me back to sleep easily, albeit with many breaks.
The day started at just after six & it followed its usual routine of Obs, pills, doctors rounds, drinks & papers in the morning, afternoons were visiting time. I was on nil by mouth, except for water, and even that was stopped at 10am because they were to schedule me for the potential back operation. At about midday a neurosurgeon visited me to discuss what other options were available, as there was some indecision about the necessity for this operation. After listening to what he had to say I insisted that Omi be brought into the discussion before anything else happened.
I'd like to say at this point that it was the morphine killing the pain for long periods that allowed me to think straight, and understand the two way conversation I needed to have with the surgeon. It is impossible to think logically and make informed decisions whilst in such pain. Immediately the op was cancelled, the angels swung into line & magically produced tea & toast ("Marmalade or jam Frank?"). Poor old Steve in the bed across just had to watch, as he was still on hold waiting to be fitted in for his operation.
On the 4th, Omi turned up, full of information & support. There was some doubt about exactly what the treatment was to be, but she was very clear that she was not in favour of major surgery as this would set back my much needed chemotherapy by some considerable time. The MRI scan needed more information gathering & many consultants seemed to be involved. There was a lot to be arranged the following day & I was sure that we had a big balancing act to follow.
Firstly was the major problem of a fast growing & aggressive small cell cancer that needed to be tackled with Chemotherapy. There was a spinal problem that had to be sorted as that could trap a nerve and stop my legs working too. There was a series of solutions for the back, ranging from major surgery, cement being injected into the vertebra or more radiotherapy. As a back up they considered a plastic back brace to help continuously support the spine.
Jan the 5th 2012 ... it's Izzy Wizzy, lets get busy!
From very early on I seemed to be up to something. I was being checked, fed & all the usual things until it was announced I was moving wards to make room for more pre-op cases.
I was taken for an early CT scan by one of the many cheerful porters, to
assess exactly where they were going to give me the radiotherapy. Before
that was to happen there was a detour. I was delivered to Occupational
Therapy to fit a white plastic all round body brace to support the back.
Wherever you go in RPH you seem to get nice staff. They were very
informative, full of smiles & most helpful. Nothing seemed to be too much
trouble & you feel you could ring anytime & be made to feel welcome &
nothing was too much bother for them. The whole thing is hand cut & "welded"
with hot water! Straps are fastened with staples & then welded into their
correct places. The inside is lined but you don't wear it next to the skin,
it goes over a T shirt. It's quite a work of art & each one is just molded
to your shape ... in my case, not too flatteringly!
It was after 3 pm before yet another happy porter whisked me off to wherever I needed go. This time it was Radiotherapy! The initial visit is always to line up the body, mark it in indelible ink to show where to give six treatments, one a day in my case. (You get a break if its weekend, of course!).
My next ward was 17 on the third floor. It's six to a room, as I had on previous stays, & this time I saw, once again, the impossible task we expect nurses & doctors to cope with.
I was the only mobile patient! I arrived to find one hard worked nurse trying to cope with the demand. Paraplegics, dementia, immobility, incontinence & often a combination of many problems. One poor man was so grateful, embarrassed but felt lost because his internal clock was completely shot at! He constantly asked for the time & followed it up with "is that morning or night?" He hated to be a nuisance but needed the toilet. Tied down by an oxygen feed and an antibiotic pump he had to be assisted but had no idea how long 5 minutes was & never stopped asking for assistance. The problem was doubled because, not only could the nurse not see to him immediately but you realise she HAS to prioritise. I bet she probably felt an inadequate and felt a failure inside her, despite knowing that she is only one angel. She knows that there aren't enough bodies to cope with the demand, too many patients & too many tasks.
As this was going on, the Prime Minister was uttering waffle about "plans" to alter the way nurses will be able to give more time to patients & do a better job. Not without more staff they can't! His plans about the top wards bringing the bottom wards up cannot be done on hot air. Politicians just want to turn up on photo opportunities in fully staffed brand new wings to show how great their system is, while the other lot just knock it all.
That night I asked about the staff. Twenty eight patients had two trained staff & two helpers. The reality seemed to be that all was fine until a problem occurred. Then they needed to prioritise as one thing set off another. Men & women, in separate bays, would be in trouble and seemed to disturb others who then wanted help. They just ran out of hands, time & practical things, like no doctor able to come at that moment, as the doctors looked after more than these 28 patients I assumed.
On the 6th, I had an excellent meeting with Mr. Hajra, register to Mr. Ray the consultant I was under about the spine problem. Because I was out of pain, I was able to discuss lucidly the way I saw my problems, what OUR priorities were to be. I was most keen that he should discuss our conversation directly with Omi, as I felt that emails to head of departments were not as effective as one to one talks. Of course I realise the work load is immense & we all need all the help we can get but this man was on my wave length & I know Omi is. I felt that both of them would do nothing but good!
So the decision was release that Friday night. Three more doses of radiotherapy, see Omi on Friday the 13th. (Good choice, Frank!!!!) Then the next set of plans can go ahead. I favour the injection of cement, as Mr. Hajra assures me it won't delay any treatment Omi wants to give me .... leave it to the experts Frank!
We were back at my son's home before tea time, so it was very successful for a Friday night I was assured.
 Forward,
trying to get the balance right.
Forward,
trying to get the balance right.
Because Cynthia took everything on her shoulders (again!) I think she got run down & developed sickness after she woke about 6 am on the Thursday. It was a bad day. She couldn't manage anything & for once I had to look after her. We finally managed to calm it down in the evening. I took advice from the local GP & afterwards rang the out of hours service who prescribed some pills & salts to drink to get her some relief. It was a rotten full day for the lass. There was no way she could come with me on my appointment with Omi the next day (13th.) Of course this meant the results of the meeting were down to my memory!!!! I made notes but there is nothing like a real live Cynthia to get it right!
It was decided to restart the Chemotherapy ASAP. That's the top priority in Omi's mind & is the most important factor in keeping me alive. She gives me the impression that once the treatment is finished & we have the back up of the radiotherapy & a back brace, then we reconsider the cement in the T7 vertebra. My next meeting will be on the 3rd February but it may not be Omi, as she is very close to her maternity leave.
Back at home, with her consent, we have reduced the morphine dosage & the back brace is proving very supportive although I'm damned glad to see the end of it at bedtime, I can tell you.
Over the weekend I developed a phlegmy chest but already had an appointment to see Dr. Renwick at our local surgery to introduce myself to the practice. He gave me antibiotics although it didn't seem to be too deeply rooted in the chest. At the same time he arranged, at the prompting of Omi, a palliative nurse, Sue, who turned up promptly on Wednesday & was most helpful & thorough. She thinks all is going well, but thought a disabled badge for the car would be of benefit. She was most kind & considerate. I'm sure we are going to get on with both her & the team of Sue Ryder nurses who are based in Keighley at their Manorlands Hospice.
 Things go down hill.
Things go down hill.
Very gradually I began to get sick in a physical way. We tried different pills & potions but we finally arrived on Friday the 3rd February to see Omi, unable to even swallow my pills without throwing up again. Sometimes I seem to be able to stave off being physically sick with either an ice lollie or a sip of milk without adverse effects. Thanks to the magic of Corn Flakes, ice cold milk & sugar, at least I'm getting some sort of goodness back inside me (OK so maybe eating the packaging would help more with the roughage. It's hardly 5 a day is it?).
Sue from Sue Ryder is proving to be be my other secret weapon. Constantly attentive by phone or visit, nothing seems ANY trouble at all. Its obvious that she & her team partner Val are going to be my advisors from now on. Sue asked us to see if we could get a chart review showing the results of all my previous blood tests to help her assess my ongoing tests, and Omi was more than happy to provide the necessary.
Omi has seen the results of the CT scan & its the end of the road for a while. No more Chemo as its having no effect on the growths, in fact they were continuing to grow whilst having it. There is another even stronger Chemotherapy but its even more toxic & I'm in no fit state to try it. At the moment my platelets are so low (they are 21 & should be between 140-450) I'm not fit to take any form of chemo anyway. Omi has told us to ask Sue to arrange weekly blood tests to keep an eye on the platelets. Apparently if the numbers go into single fingers an infusion would be necessary.
Omi has also prescribed some high dose steroids to try and help with the sickness, so we'll keep our fingers crossed there.
We are going back to meet our new oncologist, Dr. Charnley, in a month on the 2nd March as Omi is off the have her new daughter very soon. She has been so good for me & kept me alive for much longer than expected. We shall be grateful to her always.
What
happens when normal life is surrounding you?
First get yourself your loved one close by & a family that will pop in & out & stop you getting bored. Have nice cheap reliable transport so you can enjoy the sunshine at the drop of a hat & you won't worry about the cost. Also, I can recommend modern technology. If you're anything like me you'll need a computer geek to fix those Smart phones & get computers talking to each other. Book all the times of tablets, potions & appointments into your phone. Alarm & remind yourself, miss nothing & forget as little as possible. There really is a lot to remember & timings to get right. (Is it to be taken before food or after?)
You'll get the horrible experiences like sickness & diarrhea or a sore throat and many things that cancer can give you. Luckily for me, its not been too often yet, just very unpleasant sometimes. It's wonderful how people like Sue bring their help & experience to back you up. It's my first time at a terminal illness, it's her job to help back you to the hilt & support you in ways you may never have known about.
After one particularly bad night of illness she had the organisational skills to co-ordinate the surgery, district nurses, sort out more alterations with the doctor & my repeat prescription & fix regular blood tests. In fact she did so much, I bet I've missed something off!!!!
Watching the NHS & Sue Ryder working together is wonderful & a joy to behold.
Epilogue
From Ian, Franks son.
The sickness had taken its toll and dads shaking was enough to throw cornflakes across the room. Hence the reason why there hadn't been an update on the page as typing was like getting double top on a dart board from half a mile away. The doctor was called and he was taken to Airedale hospital in Keighley where he was diagnosed with renal failure. They worked quickly to put fluids in to try and kick start his system but after 24hours there was no improvement. There was nothing left but to make him confortable and let nature take its course.
They found a bed in a lovely hospice called Manorlands Sue Ryder Hospice in Keighley for him. Cynthia was by his side all the time looking after him. He was made comfortable and wasn't in any pain.
Gradually he spent more time a sleep and less time 'with it' until he finally passed away peacefully in his sleep on Sunday 19th Feb 2012 at 1.30am.
We will all miss him terribly and his wonderful sense of humour. We are all pleased he didn't suffer for long.
If you would like to donate in his memory to his favourite charities: Sue Ryder and Rosemere Cancer
Frank's Granddaughter, Amy wanted to leave her thoughts about Frank and you can read them here.
